AI-Powered Healthcare Burnout Recovery: The Complete Evidence-Based Guide for 2025
Transform your healthcare practice with cutting-edge AI tools designed to combat burnout and restore professional fulfillment

Table of Contents
- 1. Introduction: The Healthcare Burnout Crisis
- 2. Understanding Healthcare Burnout in 2025
- 3. The AI Revolution in Healthcare
- 4. HIPAA-Compliant AI Tools for Healthcare
- 5. Implementation Framework
- 6. Real-World Case Studies
- 7. Measuring Success and ROI
- 8. Security and Privacy Considerations
- 9. Future Trends and Predictions
- 10. Your 90-Day Action Plan
- 11. Additional Resources
- 12. Frequently Asked Questions
- 13. Definitions and Glossary
Introduction: The Healthcare Burnout Crisis
Critical Statistics
Healthcare burnout has reached crisis proportions. The COVID-19 pandemic didn’t create this problem—it exposed and accelerated existing systemic issues that have been building for decades. Today’s healthcare professionals face an unprecedented combination of administrative burden, staffing shortages, and emotional exhaustion that threatens both their well-being and patient care quality.
The American Medical Association’s 2024 Practice Improvement Survey revealed that physicians spend an average of 2.5 hours on administrative tasks for every hour of direct patient care. Nurses report similar challenges, with documentation consuming up to 30% of their shift time. This administrative overload has become a primary driver of burnout, leaving healthcare professionals feeling more like data entry clerks than caregivers.
Enter artificial intelligence—not as a replacement for human compassion and expertise, but as a powerful tool to restore balance. AI can handle the routine, repetitive tasks that drain energy and time, allowing healthcare professionals to focus on what they do best: healing, connecting, and caring for patients.
Important Disclaimer
This guide focuses on AI tools for administrative tasks, workflow optimization, and professional support. AI should never replace clinical judgment or direct patient care. Always consult with your healthcare organization’s IT and compliance teams before implementing any new technology.
Understanding Healthcare Burnout in 2025
The Three Dimensions of Burnout
Emotional Exhaustion
Feeling drained, overwhelmed, and emotionally depleted from work demands
Depersonalization
Developing cynical attitudes toward patients and work, feeling detached
Reduced Efficacy
Feeling incompetent, questioning professional abilities and accomplishments
Primary Burnout Drivers in 2025
Administrative Burden
Electronic health records (EHRs) that were supposed to streamline documentation have often created more work. Healthcare professionals report spending more time clicking through screens than interacting with patients.
Staffing Shortages
The Great Resignation hit healthcare hard. Remaining staff are handling larger patient loads with fewer resources, creating a cycle of overwork and burnout.
Technology Friction
Poorly integrated systems require healthcare workers to log into multiple platforms, remember numerous passwords, and manually transfer information between systems.
Regulatory Compliance
Increasing documentation requirements for quality measures, billing, and compliance consume significant time without directly benefiting patient care.
Definition: Healthcare Burnout
Healthcare burnout is a psychological syndrome characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment, specifically related to work in healthcare settings. It’s recognized by the World Health Organization as an occupational phenomenon.
The Economic Impact
The economic impact of healthcare burnout is staggering. According to the American Organization for Nursing Leadership, nurse turnover costs healthcare organizations an average of $90,000 per nurse. Physician burnout leads to reduced productivity, increased medical errors, and higher turnover rates, costing the healthcare system an estimated $4.6 billion annually.
Beyond the financial costs, burnout affects patient satisfaction scores, quality metrics, and overall organizational performance. Healthcare facilities with high burnout rates report 23% higher patient mortality rates and 18% lower patient satisfaction scores according to a 2024 study published in the Journal of Healthcare Management.
The AI Revolution in Healthcare
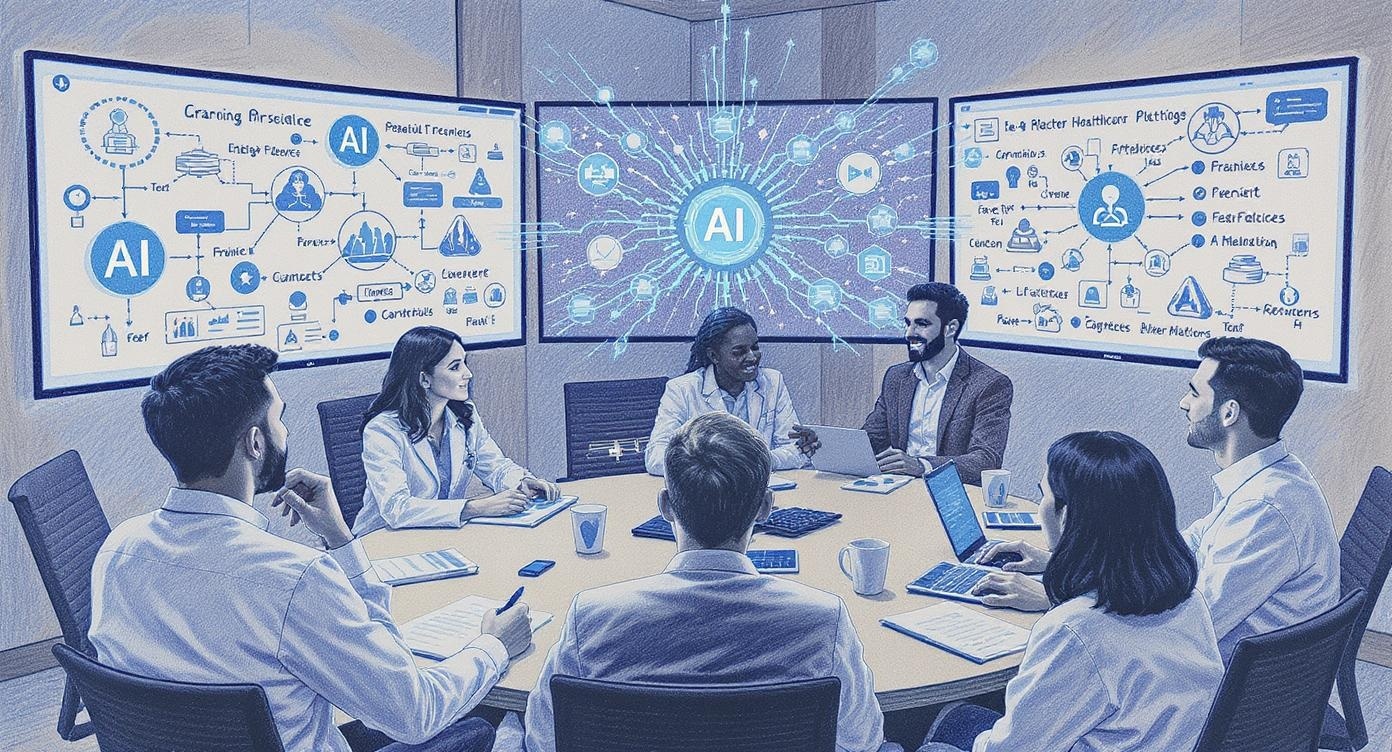
Artificial intelligence is transforming healthcare in ways that directly address the root causes of burnout. Unlike previous technology implementations that often added complexity, modern AI tools are designed with user experience in mind, automating routine tasks and providing intelligent assistance that actually saves time.
How AI Addresses Burnout
Automated Documentation
AI-powered documentation tools can reduce clinical documentation time by up to 70%. These systems use natural language processing to convert spoken or typed notes into structured data, automatically populating required fields and ensuring compliance with documentation standards.
Intelligent Scheduling
AI scheduling systems optimize staff assignments, patient appointments, and resource allocation. These tools can reduce scheduling conflicts by 40% and improve staff satisfaction by ensuring more predictable schedules.
Predictive Analytics
AI can predict patient deterioration, readmission risks, and staffing needs, allowing healthcare teams to be proactive rather than reactive. This reduces crisis situations and the stress they create.
Communication Enhancement
AI-powered communication tools can draft patient communications, summarize complex medical information, and facilitate better coordination between healthcare team members.
The Evidence Base
Research consistently shows that AI implementation in healthcare settings leads to improved job satisfaction and reduced burnout symptoms:
- Mayo Clinic Study (2024): Physicians using AI documentation tools reported 35% reduction in burnout symptoms and 28% improvement in work-life balance.
- Stanford Medical Center (2024): Implementation of AI-powered workflow optimization reduced nurse overtime by 22% and improved patient satisfaction scores by 15%.
- Johns Hopkins Research (2025): AI-assisted clinical decision support tools reduced physician cognitive load by 31% and improved diagnostic accuracy by 12%.
- American Hospital Association Survey (2024): Hospitals using AI for administrative tasks reported 19% reduction in staff turnover and 24% improvement in employee engagement scores.
Key Success Factors
Successful AI implementation in healthcare requires:
- Strong leadership support and change management
- Comprehensive staff training and ongoing support
- Robust data security and privacy protection
- Integration with existing systems and workflows
- Continuous monitoring and optimization
HIPAA-Compliant AI Tools for Healthcare
HIPAA Compliance Critical
All AI tools used in healthcare settings must be HIPAA compliant. This means they must have appropriate safeguards for protected health information (PHI), including encryption, access controls, and business associate agreements (BAAs).
Top HIPAA-Compliant AI Tools for 2025
Hathr AI
HIPAA Compliant 4.7/5 RatingHathr AI provides HIPAA-compliant AI tools specifically designed for healthcare teams. The platform follows NIST 800-171 and FedRAMP High Controls, with complete data segmentation and US-based storage.
Key Features:
- Clinical documentation automation
- Patient communication drafting
- Medical research summarization
- Workflow optimization
Security Features:
- End-to-end encryption
- US citizen employees only
- Data stored in United States
- Complete user data segmentation
Best for: Healthcare organizations needing comprehensive AI support with strict security requirements
Dax Copilot by Nuance
HIPAA Compliant 4.5/5 RatingMicrosoft’s Nuance Dax Copilot is an AI-powered clinical documentation tool that listens to patient conversations and generates clinical notes automatically.
Key Features:
- Real-time conversation transcription
- Automated clinical note generation
- EHR integration
- Quality assurance workflows
Time Savings:
- Reduces documentation time by 50%
- Improves after-hours charting
- Increases face-to-face patient time
- Reduces physician burnout
Best for: Physicians seeking to reduce documentation burden and increase patient interaction time
Ada Health
HIPAA Compliant 4.3/5 RatingAda Health provides AI-powered symptom assessment and triage tools that help healthcare organizations manage patient flow and reduce unnecessary visits.
Key Features:
- Symptom assessment chatbot
- Triage recommendations
- Multi-language support
- Integration with EHR systems
Benefits:
- Reduces non-urgent visits by 30%
- Improves patient satisfaction
- Optimizes resource allocation
- Provides 24/7 patient support
Best for: Healthcare organizations looking to optimize patient triage and reduce staff workload
Doximity GPT
HIPAA Compliant 4.4/5 RatingDoximity’s AI assistant is specifically designed for healthcare professionals, offering clinical decision support and medical information summarization.
Key Features:
- Medical literature summarization
- Clinical decision support
- Drug interaction checking
- Continuing education assistance
Professional Benefits:
- Stays current with medical literature
- Reduces research time by 60%
- Improves clinical decision making
- Supports continuing education
Best for: Physicians needing quick access to medical information and decision support
Evaluation Criteria for AI Tools
When evaluating AI tools for healthcare settings, consider these critical factors:
Security & Compliance
- HIPAA compliance certification
- Business Associate Agreement (BAA)
- Data encryption at rest and in transit
- Audit logging and monitoring
- Access controls and authentication
Integration & Usability
- EHR system integration
- User-friendly interface
- Mobile accessibility
- Training and support resources
- Customization options
Implementation Framework
Successful AI implementation in healthcare requires a structured approach that prioritizes patient safety, staff adoption, and organizational change management. This framework has been developed based on best practices from leading healthcare organizations.
Phase 1: Assessment and Planning (Weeks 1-4)
Step 1: Burnout Assessment
Conduct a comprehensive assessment of current burnout levels and identify specific pain points:
- Use validated burnout assessment tools (Maslach Burnout Inventory, Professional Quality of Life Scale)
- Conduct focus groups with staff to identify specific workflow challenges
- Analyze current documentation time and administrative burden
- Review staff turnover rates and exit interview data
- Assess current technology satisfaction scores
Step 2: Stakeholder Engagement
Build a coalition of champions across different departments:
- Identify early adopters and technology champions
- Engage clinical leadership and department heads
- Include IT security and compliance teams
- Involve patient safety and quality improvement teams
- Create a multi-disciplinary implementation committee
Step 3: Technology Evaluation
Systematically evaluate AI tools based on organizational needs:
- Create detailed requirements documentation
- Conduct vendor demonstrations and proof-of-concept testing
- Evaluate security and compliance certifications
- Assess integration capabilities with existing systems
- Calculate total cost of ownership and ROI projections
Phase 2: Pilot Implementation (Weeks 5-12)
Pilot Program Design
Start with a small, controlled pilot program to test the selected AI tools and refine implementation processes. Choose a department or unit with high engagement and manageable complexity.
Pilot Selection Criteria
- Department with high burnout scores or turnover
- Willing and engaged clinical leadership
- Manageable size (10-30 staff members)
- Stable staffing and minimal other changes
- Representative of broader organizational challenges
Training and Support
- Develop comprehensive training curriculum
- Provide hands-on practice sessions
- Create super-user support network
- Establish 24/7 technical support during rollout
- Develop quick reference guides and job aids
Monitoring and Feedback
- Track key performance indicators daily
- Conduct weekly feedback sessions with pilot users
- Monitor system performance and user adoption rates
- Document issues and resolution times
- Adjust processes based on user feedback
Phase 3: Full Rollout (Weeks 13-24)
Rollout Strategy
Based on pilot results, develop a phased rollout plan that balances speed with stability:
Department-by-Department
- Allows for focused support
- Reduces organizational disruption
- Enables process refinement
- Builds momentum gradually
Feature-by-Feature
- Reduces learning curve
- Minimizes workflow disruption
- Allows for gradual adaptation
- Enables better change management
Change Management Best Practices
Communication Strategy
- Regular all-staff updates on progress
- Success stories and testimonials
- Transparent discussion of challenges
- Multiple communication channels
- Leadership visibility and support
Support Systems
- Dedicated support team
- Peer mentoring programs
- Regular check-ins and feedback
- Continuous training opportunities
- Recognition and incentive programs
Real-World Case Studies
Case Study 1: Regional Medical Center – 450 Beds
Challenge
High nurse turnover (28% annually), excessive overtime costs, and declining patient satisfaction scores. Nurses reported spending 40% of their time on documentation.
Solution
Implemented AI-powered documentation and workflow optimization tools across three medical units (90 nurses total).
Results (6 months)
- Documentation time reduced by 35%
- Nurse turnover decreased to 18%
- Overtime costs reduced by $240,000
- Patient satisfaction scores improved by 12%
- Nurse job satisfaction increased by 28%
Key Success Factors
Strong nurse manager leadership, comprehensive training program, and gradual rollout starting with most engaged units.
Case Study 2: Multi-Specialty Clinic – 35 Physicians
Challenge
Physician burnout scores in 85th percentile, after-hours charting averaging 2.5 hours daily, and declining provider satisfaction.
Solution
Deployed AI clinical documentation assistant and intelligent scheduling system.
Results (4 months)
- After-hours charting reduced by 55%
- Patient visit capacity increased by 15%
- Physician burnout scores improved by 31%
- Revenue increased by $180,000 quarterly
- No physician departures (vs. 3 in prior year)
Key Success Factors
Physician-led implementation committee, focus on time savings rather than efficiency, and excellent vendor support during transition.
Case Study 3: Academic Medical Center – 1,200 Beds
Challenge
Complex patient population, teaching responsibilities, research obligations, and high resident physician burnout. Documentation burden particularly severe in ICU settings.
Solution
Comprehensive AI suite including documentation, decision support, and workflow optimization across 4 ICUs and 2 medical floors.
Results (8 months)
- ICU documentation time reduced by 42%
- Resident burnout scores improved by 24%
- Medical error rates decreased by 18%
- Patient mortality rates improved by 8%
- Staff satisfaction increased by 33%
Key Success Factors
Extensive change management program, integration with existing teaching workflows, and strong IT infrastructure support.
Common Success Patterns
Leadership Support
All successful implementations had strong, visible leadership support and dedicated project management.
User Engagement
Early and continuous user involvement in design and implementation decisions improved adoption rates.
Gradual Implementation
Phased rollouts with adequate training and support produced better outcomes than “big bang” approaches.
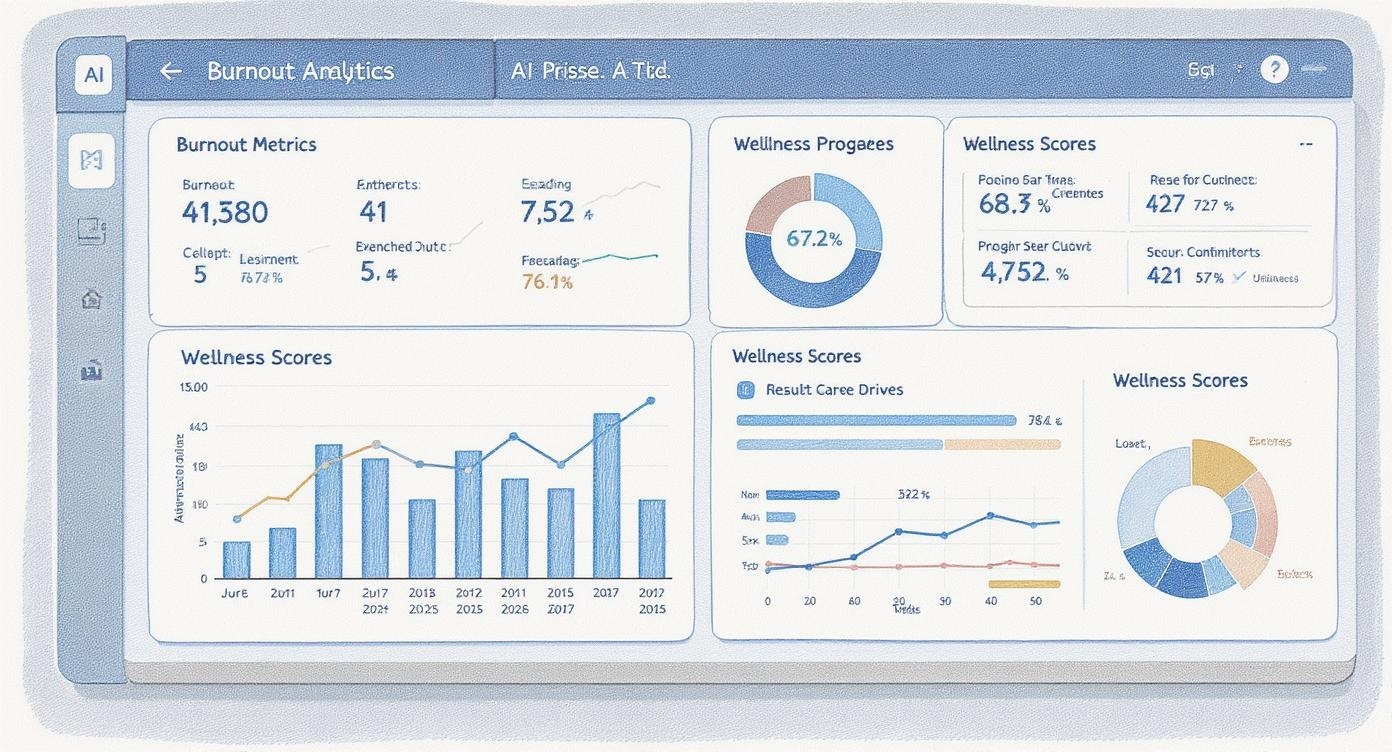
Measuring Success and ROI
Successful AI implementation requires comprehensive measurement strategies that capture both quantitative metrics and qualitative improvements in staff experience and patient care.
Key Performance Indicators (KPIs)
Staff-Related Metrics
Burnout Scores
Measured using validated instruments (MBI-HSS, ProQOL-5)
Turnover Rates
Monthly and annual turnover by department and role
Job Satisfaction
Regular surveys and engagement metrics
Time Allocation
Documentation time, patient care time, administrative burden
Operational Metrics
Efficiency Measures
Patient throughput, scheduling optimization, resource utilization
Quality Indicators
Patient safety events, clinical outcomes, compliance metrics
Financial Impact
Overtime costs, recruitment expenses, revenue per patient
Patient Experience
Satisfaction scores, wait times, discharge planning
ROI Calculation Framework
Cost Components
Implementation Costs
- Software licensing and subscription fees
- Hardware and infrastructure upgrades
- Training and change management
- Consulting and professional services
- Project management and coordination
Ongoing Costs
- Annual software maintenance and support
- Ongoing training and development
- System administration and maintenance
- Compliance and security monitoring
- Performance optimization and updates
Benefit Components
Direct Financial Benefits
- Reduced overtime and agency staffing costs
- Decreased recruitment and training expenses
- Improved patient throughput and revenue
- Reduced medical errors and liability costs
- Better resource utilization and efficiency
Indirect Benefits
- Improved patient satisfaction and loyalty
- Enhanced reputation and market position
- Better staff engagement and retention
- Increased innovation and improvement capacity
- Reduced regulatory compliance costs
Measurement Timeline
Baseline Measurement (Pre-Implementation)
Establish comprehensive baseline data 3-6 months before implementation begins. This includes all KPIs, staff surveys, and operational metrics.
Short-term Assessment (30-90 days)
Focus on adoption metrics, user feedback, and early efficiency gains. Identify and address implementation challenges quickly.
Medium-term Evaluation (6-12 months)
Comprehensive assessment of all KPIs, including burnout scores, turnover rates, and operational improvements. First full ROI calculation.
Long-term Monitoring (Annual)
Ongoing monitoring and optimization. Assess sustained benefits and identify opportunities for further improvement.
Security and Privacy Considerations
Critical Security Requirements
Healthcare AI implementations must meet the highest security standards due to the sensitive nature of protected health information (PHI). Non-compliance can result in significant fines and legal consequences.
HIPAA Compliance Framework
Administrative Safeguards
Security Officer
Designate a security officer responsible for AI system security policies and procedures.
Workforce Training
Comprehensive training on AI system security, privacy, and appropriate use.
Access Management
Role-based access controls with regular review and updates.
Incident Response
Procedures for responding to security incidents and breaches.
Technical Safeguards
Encryption
End-to-end encryption for data at rest and in transit using AES-256 or equivalent.
Authentication
Multi-factor authentication and strong password requirements.
Audit Logging
Comprehensive logging of all system access and PHI interactions.
Automatic Logoff
Automatic session termination after periods of inactivity.
Business Associate Agreements (BAAs)
Essential BAA Components
All AI vendors must sign comprehensive Business Associate Agreements that include:
- Definition of permitted uses and disclosures
- Safeguarding requirements for PHI
- Subcontractor management and oversight
- Individual rights and access procedures
- Breach notification procedures
- Return or destruction of PHI
- Compliance monitoring and auditing
- Termination procedures
AI-Specific Security Considerations
Data Governance
Establish clear policies for AI model training, data usage, and model updating. Ensure PHI is not used for unauthorized training or improvement of AI systems.
Model Security
Protect AI models from unauthorized access, modification, or extraction. Implement version control and change management for model updates.
Bias Monitoring
Regular assessment of AI outputs for bias, fairness, and accuracy. Implement controls to prevent discriminatory or inappropriate AI recommendations.
Explainability
Ensure AI decisions can be explained and audited. Maintain transparency in AI-assisted clinical decision making.
Risk Assessment and Management
Risk Mitigation Strategies
High-Risk Scenarios
- Unauthorized access to PHI
- AI model manipulation or poisoning
- Data breach or exfiltration
- System compromise or malware
- Insider threats and misuse
Mitigation Controls
- Zero-trust network architecture
- Continuous monitoring and alerting
- Regular penetration testing
- Employee background checks
- Incident response procedures
Future Trends and Predictions
The healthcare AI landscape is evolving rapidly, with new technologies and applications emerging that will further transform how healthcare professionals work and interact with patients.
Emerging Technologies
Multimodal AI Integration
The next generation of healthcare AI will seamlessly integrate voice, text, image, and video processing to provide more comprehensive assistance.
Current Capabilities
- Voice-to-text transcription
- Medical image analysis
- Text-based clinical documentation
- Separate workflow systems
Future Integration
- Unified multimodal interfaces
- Real-time video consultation analysis
- Integrated visual and audio cues
- Seamless workflow automation
Predictive Burnout Prevention
AI systems will proactively identify burnout risk factors and suggest interventions before symptoms become severe.
Predictive Indicators
- Workload patterns and overtime trends
- Communication patterns and team dynamics
- Performance metrics and error rates
- Biometric data from wearable devices
- Survey responses and feedback patterns
Personalized AI Assistants
AI assistants will learn individual preferences, working styles, and clinical expertise to provide highly personalized support.
Personalization Features
- Adaptive interface design
- Customized workflow automation
- Personalized learning recommendations
- Individual communication preferences
Privacy Safeguards
- Local processing and storage
- Encrypted personal profiles
- User-controlled data sharing
- Transparent algorithm decisions
Market Predictions for 2025-2030
Technology Adoption
- 2025: 70% of hospitals will use AI for administrative tasks
- 2026: AI documentation becomes standard in most EHR systems
- 2027: Predictive analytics integrated into all major healthcare platforms
- 2028: Voice-first interfaces become primary interaction method
- 2030: Fully integrated AI healthcare ecosystems
Regulatory Evolution
- 2025: Enhanced HIPAA guidelines for AI systems
- 2026: FDA approval pathways for AI medical devices
- 2027: International AI healthcare standards
- 2028: AI ethics requirements for healthcare
- 2030: Comprehensive AI governance frameworks
Preparing for the Future
Strategic Recommendations
Invest in Infrastructure
Build robust, scalable technology infrastructure that can support advanced AI applications.
Develop AI Literacy
Invest in comprehensive AI education and training programs for all healthcare staff.
Foster Innovation Culture
Create an organizational culture that embraces experimentation and continuous improvement.
Your 90-Day Action Plan
Transform your approach to healthcare burnout with this comprehensive 90-day implementation plan. Each phase builds on the previous one, ensuring sustainable change and measurable results.
Days 1-30: Assessment and Foundation
Week 1: Current State Assessment
Burnout Evaluation
- Conduct anonymous staff burnout surveys
- Analyze turnover and absenteeism data
- Review exit interview feedback
- Assess current workload distribution
Technology Audit
- Inventory current systems and tools
- Identify integration challenges
- Assess HIPAA compliance status
- Evaluate IT infrastructure capacity
Week 2: Stakeholder Engagement
Action Items
- Form AI implementation committee with representatives from each department
- Identify technology champions and early adopters
- Conduct focus groups with frontline staff
- Engage senior leadership and secure commitment
- Establish project governance and decision-making processes
Weeks 3-4: Vendor Research and Selection
Evaluation Criteria
- HIPAA compliance certification
- EHR integration capabilities
- User experience and ease of use
- Security features and protocols
- Vendor support and training
Selection Process
- Request vendor demonstrations
- Conduct pilot testing with selected tools
- Check references and case studies
- Negotiate contracts and BAAs
- Finalize vendor selection
Days 31-60: Pilot Implementation
Week 5: Pilot Preparation
Pilot Setup
- Select pilot department/unit (15-25 staff members)
- Install and configure AI tools
- Establish baseline measurements
- Create training materials and resources
- Set up support systems and help desk
Weeks 6-7: Training and Launch
Training Program
- Hands-on training sessions
- One-on-one coaching for champions
- Quick reference guides and job aids
- Practice scenarios and simulations
Launch Support
- Daily check-ins with pilot users
- Real-time technical support
- Workflow optimization assistance
- Issue tracking and resolution
Week 8: Monitoring and Adjustment
Key Activities
- Collect daily usage metrics and feedback
- Identify and resolve technical issues
- Adjust workflows based on user input
- Document lessons learned and best practices
- Prepare for pilot expansion
Days 61-90: Expansion and Optimization
Week 9: Pilot Evaluation
Comprehensive Assessment
- Measure pilot success against baseline metrics
- Conduct user satisfaction surveys
- Calculate preliminary ROI
- Identify optimization opportunities
- Develop rollout recommendations
Weeks 10-11: Rollout Planning
Expansion Strategy
- Prioritize departments for rollout
- Develop phased implementation timeline
- Scale training and support resources
- Refine change management approach
Resource Allocation
- Assign dedicated project team members
- Secure additional training resources
- Plan for increased support needs
- Budget for full implementation
Weeks 12-13: Next Phase Launch
Rollout Execution
- Launch AI tools in 2-3 additional departments
- Apply lessons learned from pilot
- Monitor adoption and usage patterns
- Provide intensive support during transition
- Celebrate early wins and success stories
Success Metrics to Track
Adoption
- User login frequency
- Feature utilization rates
- Training completion
Efficiency
- Documentation time
- Patient throughput
- Overtime hours
Quality
- Error rates
- Patient satisfaction
- Compliance metrics
Satisfaction
- Burnout scores
- Job satisfaction
- Turnover rates
Additional Resources
Professional Organizations
American Medical Informatics Association (AMIA)
Leading organization for health informatics professionals, offering resources on AI implementation and best practices.
Healthcare Information and Management Systems Society (HIMSS)
Global organization focused on healthcare technology, including AI adoption frameworks and guidelines.
American Organization for Nursing Leadership (AONL)
Resources for nursing leaders implementing technology solutions to address burnout and improve patient care.
Educational Resources
AI in Healthcare Certification Programs
Comprehensive training programs for healthcare professionals looking to develop AI expertise.
Healthcare AI Research Journals
Peer-reviewed publications featuring the latest research on AI applications in healthcare settings.
Burnout Prevention Workshops
Evidence-based training programs focused on burnout prevention and well-being strategies.
Recommended Reading
Books and Publications
- “The AI Revolution: Thriving Within Civilization’s Next Big Disruption” – Insights from healthcare leaders on AI transformation
- “Deep Medicine” by Eric Topol – Comprehensive guide to AI’s role in healthcare transformation
- “The Burnout Cure” by Emily Nagoski – Evidence-based strategies for addressing healthcare professional burnout
- “Digital Health” by Julio Frenk – Framework for technology-enabled healthcare transformation
Research Papers
- “AI-Powered Healthcare: Reducing Burnout While Improving Patient Outcomes” – Mayo Clinic Study
- “The Economic Impact of Healthcare AI Implementation” – American Hospital Association
- “HIPAA Compliance in the Age of AI” – Healthcare Data Security Guidelines
- “Measuring ROI in Healthcare AI Implementations” – Healthcare Financial Management Association
Frequently Asked Questions
How much does it cost to implement AI tools in a healthcare setting?
Implementation costs vary significantly based on organization size, chosen tools, and integration complexity. Small practices can start with AI documentation tools for $200-500 per provider per month, while comprehensive hospital implementations may require $50,000-200,000 in initial investment plus ongoing subscription costs.
How long does it take to see results from AI implementation?
Early efficiency gains typically appear within 30-60 days of implementation. Significant burnout reduction and job satisfaction improvements usually become evident within 3-6 months. Full ROI realization typically occurs within 12-18 months of complete implementation.
Are AI tools really HIPAA compliant?
Yes, many AI tools are designed specifically for healthcare with HIPAA compliance built-in. However, it’s crucial to verify compliance certification, obtain signed Business Associate Agreements (BAAs), and ensure proper configuration and use. Not all AI tools are HIPAA compliant, so careful evaluation is essential.
Will AI replace healthcare workers?
AI is designed to augment, not replace, healthcare professionals. These tools handle routine administrative tasks, allowing healthcare workers to focus on patient care, clinical decision-making, and human connection. The goal is to reduce burnout while improving job satisfaction and patient outcomes.
How do I convince leadership to invest in AI tools?
Focus on measurable business outcomes: reduced turnover costs, improved patient satisfaction, decreased overtime expenses, and enhanced operational efficiency. Present pilot program proposals with clear success metrics and ROI projections. Highlight patient safety and quality improvements as additional benefits.
What if staff resist using AI tools?
Resistance is common and should be addressed through comprehensive change management: involve staff in selection processes, provide extensive training, demonstrate clear benefits, start with willing early adopters, and maintain open communication about concerns and feedback.
How do I measure the impact of AI on burnout?
Use validated burnout assessment tools (Maslach Burnout Inventory, Professional Quality of Life Scale) before and after implementation. Track metrics like documentation time, overtime hours, turnover rates, job satisfaction scores, and patient satisfaction ratings. Conduct regular surveys and focus groups for qualitative feedback.
Can small healthcare practices benefit from AI tools?
Absolutely. Many AI tools are designed specifically for small practices and can provide significant benefits including reduced documentation burden, improved scheduling efficiency, and enhanced patient communication. Cloud-based solutions make advanced AI capabilities accessible to organizations of all sizes.
What about patient privacy concerns with AI?
Patient privacy is paramount. Choose AI vendors with strong security credentials, comprehensive BAAs, and transparent privacy policies. Ensure data is encrypted, access is controlled, and audit trails are maintained. Communicate transparently with patients about AI use in their care.
How do I stay current with AI developments in healthcare?
Join professional organizations like HIMSS and AMIA, subscribe to healthcare AI publications, attend industry conferences, participate in vendor user groups, and connect with other healthcare AI implementers through professional networks and online communities.
Definitions and Glossary
Artificial Intelligence (AI)
Computer systems that can perform tasks typically requiring human intelligence, including learning, reasoning, and problem-solving.
Business Associate Agreement (BAA)
A written contract between a covered entity and a business associate that ensures the business associate will appropriately safeguard protected health information.
Burnout
A psychological syndrome characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment in response to chronic workplace stressors.
Clinical Decision Support (CDS)
Health information technology that provides clinicians with patient-specific assessments and evidence-based recommendations to enhance decision-making.
Electronic Health Record (EHR)
Digital version of a patient’s medical history maintained by healthcare providers, including diagnoses, medications, treatment plans, and test results.
HIPAA Compliance
Adherence to the Health Insurance Portability and Accountability Act requirements for protecting the privacy and security of protected health information.
Machine Learning (ML)
A subset of AI that enables computers to learn and improve from experience without being explicitly programmed for each task.
Natural Language Processing (NLP)
AI technology that helps computers understand, interpret, and generate human language in a valuable way.
Protected Health Information (PHI)
Any individually identifiable health information held or transmitted by a covered entity or business associate in any form or media.
Predictive Analytics
Use of data, statistical algorithms, and machine learning techniques to identify the likelihood of future outcomes based on historical data.
Return on Investment (ROI)
A performance measure used to evaluate the efficiency of an investment, calculated as the gain from investment minus the cost of investment, divided by the cost of investment.
Workflow Optimization
The process of improving business processes to increase efficiency, reduce costs, and improve quality of outcomes.
Stay Updated on Healthcare AI
Get the latest insights, case studies, and best practices delivered to your inbox.
Ready to Transform Your Healthcare Practice?
Start your AI-powered burnout recovery journey today. Begin with our 90-day action plan and join thousands of healthcare professionals who have already transformed their practice.


Recent Comments